Modafinil for Dysautonomia: Benefits, Risks, and What the Evidence Shows
Fatigue and brain fog are two of the most disabling symptoms for people with autonomic nervous system disorders. Some patients and clinicians have considered modafinil as a way to manage these issues. Modafinil is approved for sleep-related conditions such as narcolepsy, obstructive sleep apnea, and shift work disorder, but its use in dysautonomia remains off-label (U.S. Food and Drug Administration [FDA], 2015).
What Is Modafinil?
Modafinil is a wakefulness-promoting medication that acts on brain pathways involving dopamine, orexin, and histamine to improve alertness (Greenblatt & Adams, 2023). The FDA has approved it for:
- Narcolepsy.
- Obstructive sleep apnea (as an add-on to standard therapy).
- Shift work sleep disorder (FDA, 2015).
Its half-life is about 15 hours, which means it should be taken early in the day to avoid sleep disruption (Greenblatt & Adams, 2023).
Doctors sometimes prescribe modafinil off-label for conditions such as multiple sclerosis fatigue or depression. Dysautonomia is another area where patients have tried it, particularly to address severe fatigue.
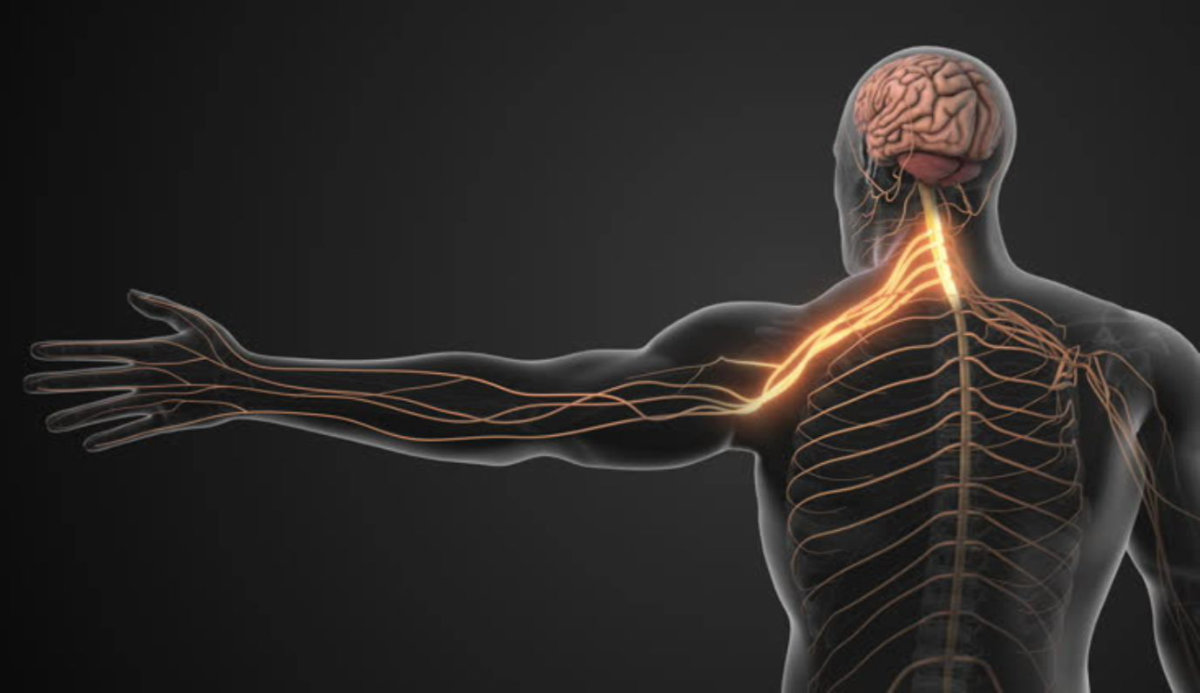
Dysautonomia and Fatigue
Dysautonomia is not a single disease but an umbrella term for conditions that affect the autonomic nervous system. Subtypes include postural orthostatic tachycardia syndrome (POTS), neurogenic orthostatic hypotension, and chronic fatigue syndrome (Benarroch, 2021). These disorders interfere with heart rate, blood pressure, and digestion. Fatigue and brain fog are among the most common and disabling symptoms (Rocha et al., 2021).
Standard treatment strategies include:
- Increasing fluid and salt intake.
- Wearing compression garments.
- Medications such as midodrine, fludrocortisone, or droxidopa.
Modafinil is not considered a first-line therapy. Instead, it may be tried as an add-on option when fatigue remains severe.
What the Evidence Shows
A randomized crossover study tested 100 mg of modafinil in patients with POTS. It found that the drug did not worsen standing heart rate or immediate orthostatic symptoms but did raise systolic blood pressure slightly (Greenblatt & Adams, 2023). This suggests short-term safety in some patients, though larger and longer studies are needed.
For chronic fatigue syndrome, evidence is inconsistent. While some clinicians report benefits, major guidelines such as those from the United Kingdom do not recommend modafinil because of limited data.
Risks and Side Effects
Like any medication, modafinil carries risks. Common side effects include:
- Headache.
- Nausea.
- Insomnia.
- Nervousness or anxiety.
Rare but serious reactions include severe rash, psychiatric symptoms, or hypersensitivity (FDA, 2015). People with liver impairment may require lower doses because modafinil is metabolized in the liver.
Drug Interactions
Modafinil affects several liver enzymes, which means it can alter the effectiveness of other medications. Important interactions include:
- Hormonal contraceptives: Modafinil reduces their effectiveness during treatment and for up to one month after stopping (FDA, 2015).
- Ivabradine and other heart rate medications: Modafinil may reduce their effectiveness because it induces the CYP3A4 enzyme.
- Other central nervous system stimulants: Combining can increase risk of overstimulation, headaches, or insomnia.
Patients should discuss all medications and supplements with their doctor before starting modafinil.
Patient Experiences
Some patients report improvements in energy and focus, allowing them to engage in daily activities more easily. Others describe only partial benefit or worsening symptoms, such as increased heart rate or disrupted sleep. Because responses vary, most patient communities recommend trying modafinil cautiously, under medical supervision, and monitoring for both benefits and side effects.
Conclusion
Modafinil may help reduce fatigue and brain fog in certain people with dysautonomia, especially those with postural orthostatic tachycardia syndrome. However, it is not approved for this purpose, and evidence remains limited. Patients should approach it as an off-label option, weigh the potential risks, and work closely with their healthcare provider to ensure safe use.
Frequently Asked Questions
Can I take modafinil at night?
No. Because modafinil has a half-life of about 15 hours, taking it late in the day can interfere with nighttime sleep (Greenblatt & Adams, 2023).
Does modafinil cure dysautonomia?
No. Modafinil may help manage fatigue and brain fog in some patients, but it does not treat the underlying cause of dysautonomia (Benarroch, 2021).
Is modafinil safe to combine with my heart medication?
It depends. Modafinil can reduce the effectiveness of drugs like ivabradine and may raise blood pressure in some people. Always consult your doctor before combining treatments (FDA, 2015).
Will modafinil affect my birth control?
Yes. Modafinil can lower the effectiveness of hormonal contraceptives during use and for up to one month after stopping. Alternative contraception is recommended (FDA, 2015).
References
- Benarroch, E. E. (2021). “Dysautonomia”: A plea for precision. Clinical Autonomic Research, 31(1), 27–29. https://doi.org/10.1007/s10286-020-00749-3
- Greenblatt, K., & Adams, N. (2023, February 6). Modafinil. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK531476/
- Rocha, E. A., Mehta, N., Távora-Mehta, M. Z. P., Roncari, C. F., Cidrão, A. A. L., & Elias Neto, J. (2021). Dysautonomia: A forgotten condition – Part 1. Arquivos Brasileiros de Cardiologia, 116(4), 814–835. https://doi.org/10.36660/abc.20200420
- U.S. Food and Drug Administration. (2015). PROVIGIL® (modafinil) tablets, for oral use, C-IV [Prescribing information]. U.S. Department of Health and Human Services. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020717s037s038lbl.pdf