What Happens If You Snort Modafinil: Risks and Effects
Modafinil is a prescription medication used to treat narcolepsy, sleep apnea, and shift work sleep disorder (Weyandt et al., 2016). Some misuse it by snorting (insufflating) the drug, believing it will produce faster or stronger effects. However, this method is ineffective and dangerous, as Modafinil is poorly water-soluble and primarily metabolized in the liver, making intranasal administration both inefficient and harmful (Robertson & Hellriegel, 2003).
Why Do Some People Snort Modafinil?
Misconceptions about Modafinil’s effects lead some users to snort it, believing that insufflation increases bioavailability and speeds up onset, similar to stimulants like cocaine or amphetamines. However, Modafinil’s pharmacokinetics do not support this (Robertson & Hellriegel, 2003; Guo et al., 2010).
- Oral administration is already highly effective, with an absorption rate of approximately 40–65% and peak plasma concentration within 1.8–2.8 hours (Robertson & Hellriegel, 2003; Guo et al., 2010).
- Snorting does not improve absorption because Modafinil is not water-soluble, making it poorly absorbed through nasal membranes (Robertson & Hellriegel, 2003).
- The liver’s metabolic processing (via the cytochrome P450 system) plays a major role in how Modafinil is activated. Snorting bypasses this pathway, likely reducing effectiveness rather than enhancing it (Guo et al., 2010).
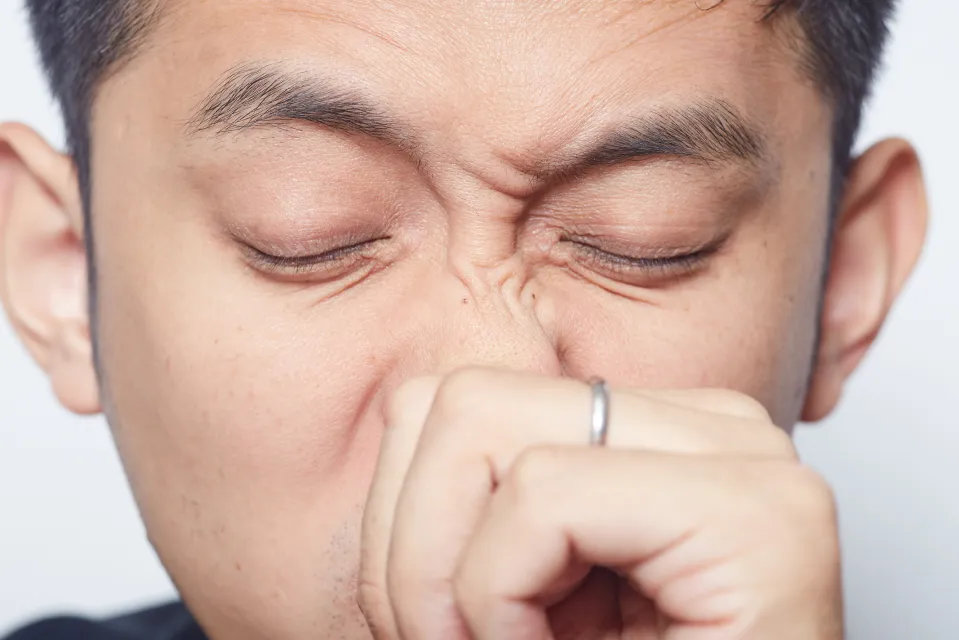
Health Risks of Snorting Modafinil
1. Damage to Nasal Passages and Sinuses
Snorting any powdered substance can cause irritation, inflammation, and potential long-term damage to the nasal and sinus tissues. Modafinil tablets contain insoluble fillers, which may contribute to nasal irritation and obstruction (Robertson & Hellriegel, 2003).
- May cause nasal congestion, bleeding, and chronic sinus infections – Snorting crushed pills introduces insoluble excipients (e.g., talc, microcrystalline cellulose), which may accumulate in nasal passages and contribute to mucosal irritation and inflammation (Robertson & Hellriegel, 2003). Chronic congestion and sinus infections have been observed in individuals who snort tablet-based medications (Peyrière et al., 2013).
- Long-term intranasal drug use has been associated with septal perforation (a hole in the nasal cartilage) – Studies on intranasal opioid and stimulant use show that prolonged exposure can lead to nasal septum damage (Peyrière et al., 2013). While there is no direct evidence for Modafinil, its tablet form and excipient content suggest a potential for similar irritation over time.
- Increased risk of respiratory infections due to damaged mucosal barriers – The nasal mucosa acts as the body’s first defense against airborne pathogens. Snorting substances that irritate or inflame these tissues may weaken this barrier, increasing susceptibility to upper respiratory infections (Alromaih et al., 2022).
2. Ineffective Absorption and Wasted Dosage
Modafinil’s insolubility in water prevents proper absorption through the nasal mucosa (Robertson & Hellriegel, 2003). Unlike drugs designed for intranasal delivery, Modafinil does not dissolve efficiently, making it poorly absorbed and largely ineffective when snorted (Tanaka et al., 2017). Much of the snorted powder ends up:
- Dripping down the throat and being swallowed, leading to delayed and unpredictable absorption (Tanaka et al., 2017).
- Being expelled when sneezing or blowing the nose, further reducing the actual dose received (Tanaka et al., 2017).
3. Increased Risk of Side Effects
Snorting Modafinil does not enhance its benefits but can amplify adverse effects due to poor absorption and unpredictable dosing (Tanaka et al., 2017). Potential side effects include:
- Severe headaches due to sinus pressure and irritation – Nasal inflammation from drug-induced rhinitis can contribute to persistent headaches and congestion (Alromaih et al., 2022).
- Dizziness and nausea from inconsistent absorption – Modafinil’s poor water solubility leads to uneven absorption, causing fluctuations in drug levels that may trigger nausea and dizziness (Tanaka et al., 2017).
- Increased heart rate and anxiety from uncontrolled dosing – Snorting Modafinil can lead to unintended overdosing, potentially causing elevated heart rate, anxiety, and blood pressure spikes (Dackis et al., 2003; Weyandt et al., 2016).
4. Potential for Misuse and Dependency
Although Modafinil has a lower abuse potential than traditional stimulants (Alromaih et al., 2022; Dackis et al., 2003), snorting drugs can reinforce risky drug-taking behaviors. Habitual misuse may:
- Lead to psychological dependency, especially in those using it for cognitive enhancement – Research suggests that individuals who misuse prescription stimulants for academic or professional performance may develop psychological reliance, even in the absence of physical addiction (Weyandt et al., 2016).
- Increase the likelihood of combining it with other substances, raising health risks – Stimulant misuse is often linked to polysubstance use, as individuals may take additional drugs to enhance euphoria or counteract side effects (Robertson & Hellriegel, 2003; Alromaih et al., 2022).
The Safest and Most Effective Way to Take Modafinil
To ensure Modafinil works as intended, it should be taken orally, as prescribed (Robertson & Hellriegel, 2003).
- Take it orally, as prescribed by a doctor – Modafinil is designed for oral administration, reaching peak plasma concentrations within 2–4 hours, making this the most effective route (Robertson & Hellriegel, 2003).
- Avoid altering the tablet (crushing, snorting, or dissolving it) – The tablet contains insoluble excipients, which may interfere with proper absorption and increase irritation risks (Robertson & Hellriegel, 2003).
- Follow proper dosage guidelines to minimize side effects – Taking Modafinil outside of recommended doses may lead to headaches, anxiety, and cardiovascular strain (Weyandt et al., 2016).
Conclusion
Snorting Modafinil is ineffective, harmful, and offers no additional benefits. The drug is designed for oral use, and attempting to bypass this can lead to nasal damage, reduced effectiveness, and increased side effects (Robertson & Hellriegel, 2003; Weyandt et al., 2016).
Anyone struggling with misuse should seek medical advice to ensure safe and responsible use.
References
- Weyandt LL, Oster DR, Marraccini ME, Gudmundsdottir BG, Munro BA, Rathkey ES, McCallum A. Prescription stimulant medication misuse: Where are we and where do we go from here? Exp Clin Psychopharmacol. 2016 Oct;24(5):400-414. doi: 10.1037/pha0000093. PMID: 27690507; PMCID: PMC5113141.
- Robertson P Jr, Hellriegel ET. Clinical pharmacokinetic profile of modafinil. Clin Pharmacokinet. 2003;42(2):123-37. doi: 10.2165/00003088-200342020-00002. PMID: 12537513.
- Guo T, Zhao LS, Xia DY. Pharmacokinetic study of modafinil in relation to gender and ethnicity in healthy young Chinese volunteers. J Pharm Pharm Sci. 2010;13(3):443-9. doi: 10.18433/j3fk5r. PMID: 21092715.
- Peyrière H, Léglise Y, Rousseau A, Cartier C, Gibaja V, Galland P. Necrosis of the intranasal structures and soft palate as a result of heroin snorting: a case series. Subst Abus. 2013;34(4):409-14. doi: 10.1080/08897077.2013.781565. PMID: 24159913.
- Alromaih S, Alsagaf L, Aloraini N, Alrasheed A, Alroqi A, Aloulah M, Alsaleh S, Alhawassi T. Drug-Induced Rhinitis: Narrative Review. Ear Nose Throat J. 2022 Nov 15:1455613221141214. doi: 10.1177/01455613221141214. Epub ahead of print. PMID: 36377650.
- Tanaka A, Furubayashi T, Enomura Y, Hori T, Shimomura R, Maeda C, Kimura S, Inoue D, Kusamori K, Katsumi H, Sakane T, Yamamoto A. Nasal Drug Absorption from Powder Formulations: Effect of Fluid Volume Changes on the Mucosal Surface. Biol Pharm Bull. 2017;40(2):212-219. doi: 10.1248/bpb.b16-00787. PMID: 28154262.
- Dackis CA, Lynch KG, Yu E, Samaha FF, Kampman KM, Cornish JW, Rowan A, Poole S, White L, O’Brien CP. Modafinil and cocaine: a double-blind, placebo-controlled drug interaction study. Drug Alcohol Depend. 2003 May 1;70(1):29-37. doi: 10.1016/s0376-8716(02)00335-6. PMID: 12681523.